Psychiatry: Is It Different? If So, How?
For centuries, the mentally ill were regarded with a combination of awe and fearful superstition, predominantly the latter. The enlightenment introduced them to humane compassion but left them subject to both isolation and faddish remedies.
The prevalence of serious mental illness in the United States now exceeds 5% of the population. Less than half of those afflicted receive minimally adequate treatment. This serious problem derives from residual stigma, unreliable availability of resources, and inequality in insurance coverage.
In recent decades, the science of psychiatry has advanced, and the field has entered the territory of evidence based medicine. But in both theory and practice, it still suffers from diagnostic vagueness and uncertainty. Partly as a result, psychiatrists confront burdensome administrative demands, and the field struggles with the heterogeneity of mental health practitioners, the majority of them outside the field of medicine.
Psychiatrists, psychologists, other licensed therapists, and their patients are thus vulnerable to discriminatory reimbursement policies. Hence, we have on-going political and social advocacy to achieve parity through education, development of effective treatment programs, and legislation.
These factors, more prevalent in psychiatry than in other medical specialties, may illuminate certain general themes in the quest for equitable and effective health care for our country. Psychiatry’s challenges may reveal certain patterns of resistance to change that might otherwise remain obscure.
Presented by:
Don Kripke, M.D.
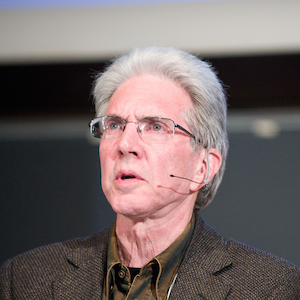
Clinical Associate Professor of Psychiatry, School of Medicine, UCSD
No slides availableNavigate the Site
2025 GoldLab Symposium
Save the date!
Please join on May 15-16, 2025Presenters In The News
Contact Info










